As a Special Olympics volunteer, your efforts are critical to achieve the Special Olympics mission and ensure that all athletes have a positive, safe and rewarding experience in Special Olympics. These guidelines are designed to protect athletes and volunteers by providing information on how to prevent emotional, sexual and physical abuse of athletes. Please take a moment to review this information carefully and ask SOAR staff if you have any questions.
Click the plus sign on the right to read more information on the following topics.
Click the plus sign on the right to read more information on the following topics.
Preventing Physical, Emotional And Sexual Abuse Of Special Olympics Athletes
Preventing Physical Abuse of Athletes
Preventing Sexual Abuse of Athletes
Identifying Signs of Abuse
In addition to statements by the athlete, there may be physical or behavioral indicators of abuse. Physical indicators include questionable injuries such as bruises, burns or lacerations in the soft tissue areas of an athlete’s body. Bruises change color during the healing process, thereby indicating that the injuries happened on more than one occasion. Injuries to genital areas may indicate sexual abuse: for example, cigarette burns on the inside of the upper leg or on the buttocks. Tether marks or rope burns and abrasions caused by tying wrists, ankles, or neck are also indicators of probable abuse.
Some athletes’ injuries are a consequence of athletic competition and the location of the injury may indicate whether the injury was due to abuse or competition. Injuries that happen during competition are most likely to be on the shins, knees, elbows, etc. They are less likely to be on the abdomen, across the back, on the backs of the legs or on facial cheeks.
If you notice that any athlete has been injured (regardless of the delegation), please ask how the injury happened. Could the incident described by the athlete have resulted in the injury you observed?
Reporting Suspected Abuse
The priority is to protect the athlete from further abuse. When an athlete discloses possible abuse to you or you have reasonable grounds to suspect that an athlete has been abused, you should also take two steps:
Step One: Contact the Authorities
Abuse, neglect and exploitation are against the law in Arkansas and so is failure to report it. If you suspect a child, a person 65 years or older, or an adult with disabilities has been abused or mistreated, you are required to report it to the DHS Division of Children and Family Services or to a law enforcement agency. You are required to make a report immediately.
Step Two: Contact Special Olympics Arkansas
Please notify your Special Olympics Arkansas area staff person immediately. If you cannot contact your area staff, please call the main office at
501-771-0222. During both calls, please inform the person you notify of the actions you have taken to protect the athlete. In addition, the athlete should be encouraged to report the abuse to the proper authorities as well.
Special Olympics Arkansas abides by the Arkansas Mandatory Reporting laws
- Do not use corporal punishment including spanking, hitting, slapping or other forms of physical discipline. Any discipline techniques used should be constructive and positive.
- Do not withhold water or food from athletes as a form of punishment. To avoid dehydration, water should be available for athletes during practice sessions, especially strenuous ones, and during competition.
- Only medications that have been prescribed by the athlete’s physician should be dispensed to that athlete, and then only as indicated on his or her athlete medical form signed by either a parent or legal guardian.
- Check to make sure water for bathing is not too hot.
Preventing Sexual Abuse of Athletes
- Do not use profanity or otherwise curse at athletes for their performance or behavior. Athletes are not to be threatened or intimidated for any purpose including attempts at improving athletic performance or for controlling behavior.
- Treat all athletes with courtesy and respect.
- Do not use demeaning nicknames or other negative or abusive language.
- Have at least two volunteers present to supervise activities such as changing into team uniforms, showering and using toilet facilities.
- When speaking privately to an athlete, volunteers should find a place out of earshot but within sight of others.
- Hugs between Special Olympics athletes and volunteers should be open to observation (not secretive) and be respectful of limits set by the athlete.
- Avoid touching areas normally covered by swimsuits: breasts, buttocks and groin. Kissing on the lips and seductive massaging is not permitted (massaging pursuant to an injury or strain is permitted, but should be open to observation by others).
- If an athlete attempts to initiate inappropriate physical contact with a volunteer, that volunteer should identify the objectionable behavior; explain that it makes him/her feel uncomfortable; and suggest more appropriate ways to communicate feelings such as “high fives” or handshakes.
- When Special Olympics events require athletes to stay overnight, the gender, age and developmental levels of the athletes should be taken into consideration when making room assignments. Athletes should also be assigned sleeping rooms with athletes of similar size and intellectual functioning. In addition, male and female athletes require separate accommodations, as well as need chaperones of their own gender.
- For all events requiring an overnight stay, the SOAR ratio of four athletes to one adult is required by gender as well, and any minor Unified Sports® partners (17 years old or younger) need to be counted with the athletes. For example, if a delegation has six male athletes, three male minor Unified Sports® partners, and five female athletes, four chaperones are needed – three male chaperones and two female chaperones.
- It is always helpful to have a sleeping chart, clearly marking which athletes are sleeping where.
- Delegation chaperones should be assigned to protect athletes anytime they are in the sleeping quarters, by ensuring that the athletes are in their assigned rooms and that any unauthorized individuals are kept out of the athletes’ sleeping quarters.
- Volunteers can assist Special Olympics staff by knowing where athletes are at all times when the athletes are in the care and custody of Special Olympics.
- All the rules of behavior should be clearly explained to the athletes before each road trip, no matter the length of the trip. Language used should be simple, but explicit.
- Information regarding trip (itinerary, hotel info, cell phone numbers for delegation leads, etc.) should be provided to all parents, guardians or caregivers prior to departing on the trip.
Identifying Signs of Abuse
In addition to statements by the athlete, there may be physical or behavioral indicators of abuse. Physical indicators include questionable injuries such as bruises, burns or lacerations in the soft tissue areas of an athlete’s body. Bruises change color during the healing process, thereby indicating that the injuries happened on more than one occasion. Injuries to genital areas may indicate sexual abuse: for example, cigarette burns on the inside of the upper leg or on the buttocks. Tether marks or rope burns and abrasions caused by tying wrists, ankles, or neck are also indicators of probable abuse.
Some athletes’ injuries are a consequence of athletic competition and the location of the injury may indicate whether the injury was due to abuse or competition. Injuries that happen during competition are most likely to be on the shins, knees, elbows, etc. They are less likely to be on the abdomen, across the back, on the backs of the legs or on facial cheeks.
If you notice that any athlete has been injured (regardless of the delegation), please ask how the injury happened. Could the incident described by the athlete have resulted in the injury you observed?
Reporting Suspected Abuse
The priority is to protect the athlete from further abuse. When an athlete discloses possible abuse to you or you have reasonable grounds to suspect that an athlete has been abused, you should also take two steps:
Step One: Contact the Authorities
Abuse, neglect and exploitation are against the law in Arkansas and so is failure to report it. If you suspect a child, a person 65 years or older, or an adult with disabilities has been abused or mistreated, you are required to report it to the DHS Division of Children and Family Services or to a law enforcement agency. You are required to make a report immediately.
Step Two: Contact Special Olympics Arkansas
Please notify your Special Olympics Arkansas area staff person immediately. If you cannot contact your area staff, please call the main office at
501-771-0222. During both calls, please inform the person you notify of the actions you have taken to protect the athlete. In addition, the athlete should be encouraged to report the abuse to the proper authorities as well.
Special Olympics Arkansas abides by the Arkansas Mandatory Reporting laws
Disclosure Of Misconduct Or Inappropriate Behavior
It is critical that behavior deemed inappropriate is disclosed to SOAR staff as soon as the behavior is witnessed or when there is an awareness that it has occurred. Below is a chart that will identify some guidelines for which behaviors are important to disclose and what steps SOAR will take related to the level of severity.
By following these guidelines, we are able to protect not only our athletes, but the integrity of the umbrella insurance coverage that is in place for all Special Olympics programs. The coverage is tied together such that one situation can jeopardize the coverage for every state.
The below referenced behaviors occurring outside an SOAR event can also be taken into consideration with regards to disciplinary action.
By following these guidelines, we are able to protect not only our athletes, but the integrity of the umbrella insurance coverage that is in place for all Special Olympics programs. The coverage is tied together such that one situation can jeopardize the coverage for every state.
The below referenced behaviors occurring outside an SOAR event can also be taken into consideration with regards to disciplinary action.
Your browser does not support viewing this document. Click here to download the document.
SO Incident Form
A Guide For Parents And Care Providers To Help Keep Our Athletes Safe
Here at Special Olympics, we believe that EVERYONE, including staff, volunteers, parents, caregivers and coaches has a role to play in ensuring the safety of Special Olympics athletes. We take this responsibility seriously and have implemented a number of steps to help make participating in Special Olympics not only rewarding, but also safe. We know that we cannot safeguard our athletes without YOUR help! We need the involvement of others, including parents and caregivers in order to be successful.
What Is Special Olympics Doing?
How Can I Help?
(1) Know what to expect from Special Olympics.
The following is a very brief overview of some of the types of official activities that are available to Special Olympics athletes
(2) Watch for “Red Flag” Behaviors:
While we cannot make a generalization that will address every possible scenario, there are certain behaviors that should raise a red flag. These include, but are not limited to:
(3) Report Suspicious Behavior
What if I Have A Concern?
If you believe a Special Olympics volunteer is engaging in activities that do not fit within the expected scope of Special Olympics, contact your Special Olympics State Program office to discuss the situation. If you believe that a Special Olympics athlete has been abused, contact law enforcement in addition to your local Special Olympics Program office, as law enforcement has the expertise to investigate such allegations.
A Guide For Parents And Care Providers To Help Keep Our Athletes Safe
Here at Special Olympics, we believe that EVERYONE, including staff, volunteers, parents, caregivers and coaches has a role to play in ensuring the safety of Special Olympics athletes. We take this responsibility seriously and have implemented a number of steps to help make participating in Special Olympics not only rewarding, but also safe. We know that we cannot safeguard our athletes without YOUR help! We need the involvement of others, including parents and caregivers in order to be successful.
What Is Special Olympics Doing?
- Volunteer Screening: Registered Volunteers who meet certain criteria, including having close contact with athletes, are screened using a national criminal background check vendor.
- Protective Behaviors Training: Registered Volunteers who have close contact with Special Olympics athletes are required to complete the Protective Behaviors training, which highlights possible signs of physical, sexual and emotional abuse so that all volunteers are active in helping us achieve our ultimate goal of protecting Special Olympics athletes from harm or abuse.
- Dating Policy: Special Olympics prohibits any staff member or volunteer (excluding spouses of Special Olympics athletes and Special Olympics athletes who are "day of event" volunteers) from dating or having a sexual relationship with any Special Olympics athlete. Exceptions may be considered by the Program’s Chief Executive Officer for athletes who are also volunteers and/or staff members.
How Can I Help?
(1) Know what to expect from Special Olympics.
The following is a very brief overview of some of the types of official activities that are available to Special Olympics athletes
- Local Level Team Practices Competitions: These practices and competitions are organized by your local Special Olympics Program or coach (individual one-on-one practices fall outside the normal scope of Special Olympics activities). Athletes are expected to arrive at the practice location at the appointed practice time and leave immediately following the conclusion of the practice, as volunteers/coaches are only present during the appointed practice times.
- State/National/Regional/World Games: Larger events organized by your Special Olympics. Program State office or Special Olympics, Inc. may require travel and/or an overnight stay(s). Parents and caregivers should request details regarding travel and housing accommodations, when applicable, and address any concerns prior to the event with their local Program office.
- Healthy Athletes®: Special Olympics athletes receive a variety of health screenings and services in a series of clinics conducted in a welcoming, fun environment. Parents/caregivers/athletes will be required to consent to such screening, if interested.
- Unified Sports®: This initiative combines approximately equal numbers of Special Olympics athletes and athletes without intellectual disabilities (Partners) on sports teams for training and competition. One outcome of Unified Sports activities may be new friendships that extend beyond official Special Olympics activities. Parents and caregivers should use their own discretion in determining an appropriate friendship level outside of official Special Olympics activities.
- Unified Champion Schools®: This initiative is an education-based project that uses sports and education programs to activate young people to develop school communities where all youth are agents of change; fostering respect, dignity and advocacy for people with intellectual disabilities. Parents and caregivers should use their own discretion in determining an appropriate level of participation/friendships outside of official Special Olympics activities.
- Athlete Leadership Programs: These programs allow athletes to explore opportunities for participation in various leadership community roles. Parents and caregivers should use their own discretion in determining appropriate community roles/activities outside of official Special Olympics activities.
- Fundraising Activities and Events: It is difficult to define "typical" fundraising involvement that parents or care providers should anticipate. It is not a requirement of Special Olympics that athletes participate in fundraising, and athletes/parents/care givers must use their own discretion in determining if and how an athlete decides to become involved in these efforts or events.
(2) Watch for “Red Flag” Behaviors:
While we cannot make a generalization that will address every possible scenario, there are certain behaviors that should raise a red flag. These include, but are not limited to:
- Inappropriate gifts, trips, outings, or other gestures of affection from a volunteer;
- Invitations for sleepovers at a volunteer’s house;
- Invitations for social events at a volunteer’s house that do not include, or specifically exclude, parents or caregivers;
- Excessive displays of interest in a particular athlete or group of athletes; and
- A Volunteer’s interest in an athlete outside the normal scope of a Special Olympics activity.
(3) Report Suspicious Behavior
What if I Have A Concern?
If you believe a Special Olympics volunteer is engaging in activities that do not fit within the expected scope of Special Olympics, contact your Special Olympics State Program office to discuss the situation. If you believe that a Special Olympics athlete has been abused, contact law enforcement in addition to your local Special Olympics Program office, as law enforcement has the expertise to investigate such allegations.
Heat Exposure
Special Olympics practices, competitions, and activities often are conducted outdoors, and we would like to provide some safety procedures to help keep everyone safe and cool. Following the simple risk management techniques outlined below can help prevent heat stroke injuries and illnesses:
- Provide consistent breaks/rest periods for all athletes and coaches.
- Make available shade/fans/cooling systems, if possible. During periods when athletes are not participating, but may be waiting on the sidelines, athletes should not sit or stand in sunshine or sit in cars without air conditioning for extended periods of time.
- Ensure there is a continuing supply of fresh drinking water at all outdoor practices and competitions.
- Have access to medical personnel on site, if possible.
- Promote the use of sunscreen and have it available.
- Ensure that athletes are wearing clothing that is loose fitting, light colored and cotton, if possible, including hats.
- Consider the Heat Index (temperature and humidity combined) and suspend competition (or practice) if heat conditions become overly oppressive or if several athletes are laboring or show any symptoms listed below.
- Avoid activities in the early and mid afternoon hours (11:00 a.m. to 2:00 p.m. is usually the hottest time of day).
- increased thirst
- headache
- dry mouth and swollen tongue
- weakness
- dizziness
- confusion
- sluggishness
- vomiting
- inability to sweat
- Sip small amounts of water (too much water too fast is not effective and may be harmful).
- Drink carbohydrate/electrolyte-containing drinks (e.g., PowerAde or Pedialyte). Carbonated soft drinks or drinks with caffeine should not be consumed.
- Suck on popsicles made from juices or sports drinks.
- Suck on ice chips.
- Sip through a straw.
- Cool water-soaked towels around the back of the neck may provide some relief.
sports injuries
Blood-Borne Contagious Infection Carriers
Special Olympics, Inc. has issued the following position regarding blood-borne contagious infection carriers:
Since medical history and examination cannot reliably identify individuals infected with HIV or other diseases, blood and body fluid precautions should be used consistently. This approach, recommended by the Centers for Disease Control and Prevention (CDC), referred to as “universal precautions,” should be used in the care of all individuals participating in Special Olympics (athletes, coaches, volunteers and staff).
Important: While the following procedures should be followed as closely as possible, emergency medical care involving blood or mouth-to-mouth contact should not be delayed due to the lack of gloves, towels or mouthpieces.
Towels
Use towels to place a barrier between yourself and blood or body fluids containing visible blood when there is no time to put on gloves. Cloth or paper towels are acceptable as long as they provide an effective barrier (thick and absorbent) to protect against direct contact with blood. Towels should be disposed of in a covered, plastic-lined container. Wash hands after handling soiled towels or linens.
Gloves
Gloves are required in the following instances:
Hand Washing
Hands must be washed immediately and thoroughly:
Studies have shown that viruses, including the HIV virus, are rapidly inactivated after being exposed to commonly used chemical germicides at concentrations that are much lower than used in practice. A diluted solution of household bleach should be prepared in the ratio of 1 to 100 which is the same as two tablespoons chlorine bleach to one gallon of water. This solution can be used for general cleaning and disinfecting purposes, and can be placed in spray bottles. All containers with bleach-water solution must be stored in a secure location.
Cleaning the Surfaces of Mats, Work and Play Areas - Wipe surfaces with a solution of chlorine bleach using a 1 to 100 ratio, dispensed from a spray bottle. Wipe or rinse with clear water. Cleaning Athletic Equipment and Toys. An easy procedure for cleaning athletic equipment and plastic toys is simply to immerse them in a chlorine bleach and water solution. Then immerse them in a container of water or spray to rinse. It is important to rinse the equipment so that the cleaning solution will not dry on the surface. They can be air dried. Porous equipment, such as wooden bats, may be dipped and rinsed immediately, but not soaked.
Laundry - Standard laundry procedures are acceptable for preventing the spread of infectious diseases.
Trash - All waste should be placed in bags and tied securely for removal.
Mouthpieces for Use in Performing CPR - Use mouthpieces for mouth-to-mouth resuscitation. Mouthpieces must be available for use in areas in which there may be a resuscitation. To disinfect the mouthpieces, wash in soap and water and disinfect in a chlorine bleach and water solution.
Procedure for Cleaning and Decontaminating Spills of Blood or Other Body Fluids
A diluted solution of household chlorine bleach and water is also acceptable for use in cleaning spills of body fluids. The solution must be made daily and containers with bleach water solution must be stored in secure locations. Gloves must be worn for this procedure.
Special Olympics, Inc. has issued the following position regarding blood-borne contagious infection carriers:
- It is not necessary nor justifiable to discriminate against any individual having ordinary behavior (behavior that does not pose a personal risk) on the basis that they are carriers of a blood-borne contagious infection.
- Under casual social interaction, carriers of a blood-borne contagious infection pose no danger to those around them; therefore, it is neither necessary nor justifiable to exclude them from participation in Special Olympics activities, nor isolate them from other participants in dormitories or sports competition.
- Participants may have a blood-borne contagious infection that is new and unknown. Therefore, universal precautions should be used for every exposure to anyone’s blood, saliva or other bodily fluid.
- Special Olympics, Inc. recommends that blood and body fluid precautions be consistently used for all people regardless of their blood-borne infection status. This practice is referred to as “universal blood and body fluid precautions” or “universal precautions.”
Since medical history and examination cannot reliably identify individuals infected with HIV or other diseases, blood and body fluid precautions should be used consistently. This approach, recommended by the Centers for Disease Control and Prevention (CDC), referred to as “universal precautions,” should be used in the care of all individuals participating in Special Olympics (athletes, coaches, volunteers and staff).
Important: While the following procedures should be followed as closely as possible, emergency medical care involving blood or mouth-to-mouth contact should not be delayed due to the lack of gloves, towels or mouthpieces.
Towels
Use towels to place a barrier between yourself and blood or body fluids containing visible blood when there is no time to put on gloves. Cloth or paper towels are acceptable as long as they provide an effective barrier (thick and absorbent) to protect against direct contact with blood. Towels should be disposed of in a covered, plastic-lined container. Wash hands after handling soiled towels or linens.
Gloves
Gloves are required in the following instances:
- Whenever you will be in contact with blood or body fluids containing visible blood.
- Whenever you are diapering a person with diarrhea.
- If you have cuts, open wounds or lesions on your hands and you will be providing services directly to an individual, such as diapering or first aid, involving body fluids.
- Change gloves between procedures which require gloves. Dispose of gloves in a plastic bag and then discard in a covered, lined container.
Hand Washing
Hands must be washed immediately and thoroughly:
- If contaminated directly with blood or body fluids (urine, feces, vomit or mucous).
- Before and after each diaper change.
- Immediately after gloves are removed.
- Before eating or handling food.
- After using the restroom.
- Accepted hand washing procedures are as follows:
- Use soap and running water.
- Rub your hands vigorously for 15 seconds.
- Wash all skin surfaces including:
- Backs of hands
- Wrists
- Between fingers
- Under fingernails
- Rinse well.
- Dry hands with a paper towel. Turn the water off with a paper towel – not with your bare hands.
- Any soap product is acceptable. If using bar soap, be sure that it is kept in a self-draining soap dish.
Studies have shown that viruses, including the HIV virus, are rapidly inactivated after being exposed to commonly used chemical germicides at concentrations that are much lower than used in practice. A diluted solution of household bleach should be prepared in the ratio of 1 to 100 which is the same as two tablespoons chlorine bleach to one gallon of water. This solution can be used for general cleaning and disinfecting purposes, and can be placed in spray bottles. All containers with bleach-water solution must be stored in a secure location.
Cleaning the Surfaces of Mats, Work and Play Areas - Wipe surfaces with a solution of chlorine bleach using a 1 to 100 ratio, dispensed from a spray bottle. Wipe or rinse with clear water. Cleaning Athletic Equipment and Toys. An easy procedure for cleaning athletic equipment and plastic toys is simply to immerse them in a chlorine bleach and water solution. Then immerse them in a container of water or spray to rinse. It is important to rinse the equipment so that the cleaning solution will not dry on the surface. They can be air dried. Porous equipment, such as wooden bats, may be dipped and rinsed immediately, but not soaked.
Laundry - Standard laundry procedures are acceptable for preventing the spread of infectious diseases.
Trash - All waste should be placed in bags and tied securely for removal.
Mouthpieces for Use in Performing CPR - Use mouthpieces for mouth-to-mouth resuscitation. Mouthpieces must be available for use in areas in which there may be a resuscitation. To disinfect the mouthpieces, wash in soap and water and disinfect in a chlorine bleach and water solution.
Procedure for Cleaning and Decontaminating Spills of Blood or Other Body Fluids
A diluted solution of household chlorine bleach and water is also acceptable for use in cleaning spills of body fluids. The solution must be made daily and containers with bleach water solution must be stored in secure locations. Gloves must be worn for this procedure.
- Remove any visible matter with disposable towels.
- Spray the surface with chlorine bleach solution. Leave the solution on the area for 10 minutes.
- Rinse with water and wipe dry.
- Dispose of gloves and paper towels in a plastic bag and discard into a covered, lined container.
First Aid Kits
All Special Olympics teams must have access to a first aid kit at all trainings, clinics, competitions, etc. All first aid kits should include:
All Special Olympics teams must have access to a first aid kit at all trainings, clinics, competitions, etc. All first aid kits should include:
|
|
Medications (prescription and nonprescription) will not be dispensed without the written consent of the parent and/or guardian of the athlete. If permission is given to dispense medication, it shall be in its original container with the athlete’s name, date, directions and physician’s name. Medications dispensed will be limited to routine oral ingestion not requiring special knowledge or skills of coaches and/or chaperones. Special Olympics encourages coaches interested in additional information to contact the American Red Cross and go through First Aid and/or CPR Training which counts toward continuing education requirements.
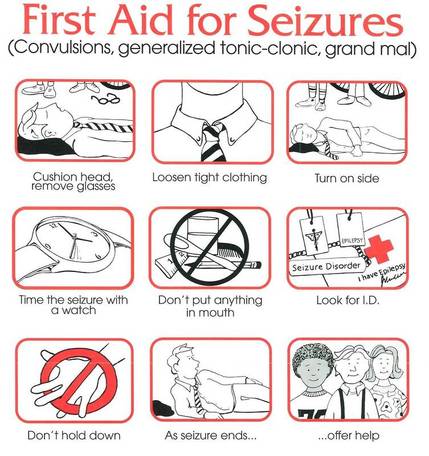
First Aid for Seizures
(Convulsions, generalized tonic-clonic, grand mal)
Although most seizures end naturally without emergency treatment, a seizure in someone who does not have epilepsy could be a sign of serious illness. Call for medical assistance if:
(Convulsions, generalized tonic-clonic, grand mal)
Although most seizures end naturally without emergency treatment, a seizure in someone who does not have epilepsy could be a sign of serious illness. Call for medical assistance if:
- seizure lasts for more than five minutes.
- no “epilepsy/seizure disorder” I.D.
- slow recovery, a second seizure, or difficult breathing afterwards.
- pregnancy or other medical I.D.
- any signs of injury.
|
If seizure lasts more then 5 minutes call 911
|
Handling Partial Seizures
Simple partial seizures don’t require any special response except to recognize what’s happening and be supportive when the seizure is over. Handling Complex Partial Seizures – the following steps may help:
|
injury prevention and treatment
What can I do to help prevent injuries?
There are two factors in preventing injuries that you should be aware of: providing a safe environment for athletes and spectators, and creating a safe work environment.
In addition to providing a safe environment for the athletes you train, you also must do your part to provide volunteers and workers with an appropriate and safe environment in which to contribute. One aspect of a safe workplace is to train personnel in proper work techniques, such as lifting, workspace ergonomics, use of tools and machinery, and defensive driving. Personnel need to become aware of workplace dangers and strive to minimize the risks, either through safe work practices or the prompt correction of hazardous situations.
What is medical emergency preparedness, and how do I prepare?
Answer the following questions to assess your preparedness for emergency medical response. The answer to all questions should be “yes.” If an answer is “no” you should take steps to address the situation.
Medical Emergency Awareness
It is the coach’s job to maintain as safe an environment as possible. It is strongly recommended that coaches have certification in CPR and First Aid or that volunteers be recruited who already have first aid training, medical athletic training or emergency care certification. Athlete medical forms should be reviewed prior to the start of practice and available at all training and competitions. There should be a plan for emergencies. Using the Coach’s Safety Check list will help to prevent injury by assuring adequate supervision, equipment, facility, warm-up and stretching.
When an injury does occur, stay calm, and administer only basic first aid. When in doubt, or when more care is needed, consult the athlete’s family and a physician.
Treating Floor Burns, Strains, Contusions, Minor Bumps and Bruises
Always have someone familiar with basic life support and cardiopulmonary resuscitation (CPR) at every training session. Even though the possibility of cardiac arrest is much greater in the spectator section than with the athletes, it is always present. Initial measures include:
SOAR Recreational Swimming Policy
There are two factors in preventing injuries that you should be aware of: providing a safe environment for athletes and spectators, and creating a safe work environment.
In addition to providing a safe environment for the athletes you train, you also must do your part to provide volunteers and workers with an appropriate and safe environment in which to contribute. One aspect of a safe workplace is to train personnel in proper work techniques, such as lifting, workspace ergonomics, use of tools and machinery, and defensive driving. Personnel need to become aware of workplace dangers and strive to minimize the risks, either through safe work practices or the prompt correction of hazardous situations.
What is medical emergency preparedness, and how do I prepare?
Answer the following questions to assess your preparedness for emergency medical response. The answer to all questions should be “yes.” If an answer is “no” you should take steps to address the situation.
Medical Emergency Awareness
- Are coaches and chaperones aware of athletes’ pre-existing medical problems, such as diabetes, epilepsy or allergic reaction to a bee sting?
- Do coaches and chaperones have ready access to the Athlete/Parent Release Forms which give permission for medical treatment in case of emergency?
- Do coaches and chaperones have these waivers available at each of the training sessions and competitions?
- Is a well-stocked first aid kit also available at the training sessions and competitions?
- Have coaches been instructed how to use the materials in the first aid kit?
- If a medical emergency occurs at a training site, do coaches know the location of the nearest telephone to call the appropriate emergency number? If that phone is in a locked room, do they have a key? Is a custodian on duty and easily found? If the phone is out of order, do they know the location of the next available phone? If it is a switchboard phone, do they know how to get an outside line?
- If a medical emergency occurs at an event or training site, are there adequate assistant coaches or volunteers available to stay with other team members while medical emergency procedures are taken?
- If a medical emergency occurs at a competition or event, does each coach and volunteer know the emergency plan: who to contact, location of contact, method of communication and follow-up procedures? Has an emergency plan been developed, and has it been included in the pre-event training of each volunteer?
- If paramedics have to be called, will they find locked gates blocking access to the injured athlete? If so, do coaches or volunteers have a key for those gates or a way to get one quickly?
- Do coaches or chaperones have a list of the names and phone numbers of the parents or group home providers to call in the event of a serious injury?
- Where is the nearest hospital to the training or competition site? Is that where an ambulance will take the injured athlete?
- * If the answer to any of these questions is “no,” coaches or volunteers are not prepared to deal with a medical emergency at an event or training site.
- Do not move an athlete who you believe may be seriously injured, especially in the case of a head, neck or back injury.
- A responsible person must stay with the injured athlete at all times and have the athlete’s Medical Release Form available.
- For a medical emergency in the United States, a responsible person should call 911 for the paramedics as quickly as possible, and go to meet them at the site entrance.
- Contact the parent or care provider as soon as possible.
- Caller’s name
- Name of site and location of its intersecting streets
- Injured athlete’s location at the site
- Type of injury
It is the coach’s job to maintain as safe an environment as possible. It is strongly recommended that coaches have certification in CPR and First Aid or that volunteers be recruited who already have first aid training, medical athletic training or emergency care certification. Athlete medical forms should be reviewed prior to the start of practice and available at all training and competitions. There should be a plan for emergencies. Using the Coach’s Safety Check list will help to prevent injury by assuring adequate supervision, equipment, facility, warm-up and stretching.
When an injury does occur, stay calm, and administer only basic first aid. When in doubt, or when more care is needed, consult the athlete’s family and a physician.
Treating Floor Burns, Strains, Contusions, Minor Bumps and Bruises
- R - Rest; stop any pain-causing activity.
- I - Ice for 24-36 hours after the injury.
- C - Compress with elastic bandage if needed.
- E - Elevate to avoid edema and subsequent swelling.
- Significant swelling or dislocation of an extremity
- Obvious deformity of an arm or leg
- Severe pain
- Inability to bear weight on a lower extremity
- Lacerations with or without fractures.
- Significant swelling of a joint (e.g., elbow, wrist, knee, ankle)
- Loss of sensation in an extremity
- Loss of consciousness
- Neck or back injury with loss of sensation or motor power in arms or legs
- Head injury with disorientation and/or visual changes
Always have someone familiar with basic life support and cardiopulmonary resuscitation (CPR) at every training session. Even though the possibility of cardiac arrest is much greater in the spectator section than with the athletes, it is always present. Initial measures include:
- Establishing unresponsiveness
- Calling out for assistance
- Positioning the victim
SOAR Recreational Swimming Policy
rehabilitation/treatment for chronic sport injuries
Blisters
Special Olympics Arkansas' Concussion Awareness and Safety Recognition Policy
It is Special Olympics Arkansas' intent to take steps to help ensure the health and safety of all Special Olympics Arkansas participants. All Special Olympics Arkansas participants should remember that safety comes first and should take reasonable steps to help minimize the risks for concussion or other serious brain injuries.
All Special Olympics Arkansas Coaches must have passed concussion training with in the past 3 years. It is recommended that all coaches carry with them Special Olympics Arkansas Concussion Education Card.
Defining a Concussion
A concussion is defined by the Centers for Disease Control as a type of traumatic brain injury caused by a bump, blow, or jolt to the head as well as serial, cumulative hits to the head. Concussions can also occur from a blow to the body that causes the head and brain to move quickly back and forth—causing the brain to bounce around or twist within the skull. Although concussions are usually not life-threatening, their effects can be serious and therefore proper attention must be paid to individuals suspected of sustaining a concussion.
Suspected or Confirmed Concussion
Participant who is suspected of sustaining a concussion in a practice, game or competition shall be removed from practice, play or competition at that time. If a qualified medical professional (advanced practice nurse, athletic trainer, physician’s assistant or physician) is available on-site to render an evaluation, that person shall have final authority as to the removal or return to play of the participant. If applicable, the participant’s parent or guardian should be made aware that the participant is suspected of sustaining a concussion.
Return to Play
A participant who has been removed from practice, play or competition due to a suspected concussion may not participate in Special Olympics Arkansas sports activities until either of the following occurs
Frequency of Training
Concussion awareness training must be completed by all Coaches at least once every three years, new coaches to Special Olympics Arkansas will go through the training as part of their certification process. Currently certified coaches will take the training upon renewing their Class A
Volunteer registration
There are two currently approved courses available for Special Olympics Arkansas coaches and the preferred one is presented free of charge on the National Federation of State High School Coaches Association. The website is: www.nfhslearn.com/courses/38000. Coaches must register and will then have access to all the online trainings. Please make sure you list Special Olympics Arkansas when filling out the School/Association line.
Communication with Parents and Guardians
The Centers for Disease Control website www.cdc.gov/concussion provides additional resources relative to concussions that may be of interest to participants and their families.
- Keep pressure off new blisters using a felt “doughnut.”
- Where the skin is torn, use extreme care.
- Keep it clean, and cut skin halfway around the perimeter without removing the skin.
- Apply antiseptic ointment and a sterile dressing.
- When underlying tissue toughens, cut away the remaining flap of skin.
- Keep them clean.
- Expose them to the air when possible.
- Keep them dry.
- Encourage gentle activity.
- Chronic rest for 5-7 days.
- Ice for pain.
- Stretch related muscles to strengthen them.
- Move gently, stopping at the point of pain.
- Exercise to strengthen afflicted area as it heals.
Special Olympics Arkansas' Concussion Awareness and Safety Recognition Policy
It is Special Olympics Arkansas' intent to take steps to help ensure the health and safety of all Special Olympics Arkansas participants. All Special Olympics Arkansas participants should remember that safety comes first and should take reasonable steps to help minimize the risks for concussion or other serious brain injuries.
All Special Olympics Arkansas Coaches must have passed concussion training with in the past 3 years. It is recommended that all coaches carry with them Special Olympics Arkansas Concussion Education Card.
Defining a Concussion
A concussion is defined by the Centers for Disease Control as a type of traumatic brain injury caused by a bump, blow, or jolt to the head as well as serial, cumulative hits to the head. Concussions can also occur from a blow to the body that causes the head and brain to move quickly back and forth—causing the brain to bounce around or twist within the skull. Although concussions are usually not life-threatening, their effects can be serious and therefore proper attention must be paid to individuals suspected of sustaining a concussion.
Suspected or Confirmed Concussion
Participant who is suspected of sustaining a concussion in a practice, game or competition shall be removed from practice, play or competition at that time. If a qualified medical professional (advanced practice nurse, athletic trainer, physician’s assistant or physician) is available on-site to render an evaluation, that person shall have final authority as to the removal or return to play of the participant. If applicable, the participant’s parent or guardian should be made aware that the participant is suspected of sustaining a concussion.
Return to Play
A participant who has been removed from practice, play or competition due to a suspected concussion may not participate in Special Olympics Arkansas sports activities until either of the following occurs
- (1) at least seven (7) consecutive days have passed since the participant was removed from play and a currently licensed, qualified medical professional provides written clearance for the participant to return to practice, play and competition or
- (2) a currently licensed, qualified medical professional determines that the participant did not suffer a concussion and provides written clearance for the participant to return to practice play immediately.
Frequency of Training
Concussion awareness training must be completed by all Coaches at least once every three years, new coaches to Special Olympics Arkansas will go through the training as part of their certification process. Currently certified coaches will take the training upon renewing their Class A
Volunteer registration
There are two currently approved courses available for Special Olympics Arkansas coaches and the preferred one is presented free of charge on the National Federation of State High School Coaches Association. The website is: www.nfhslearn.com/courses/38000. Coaches must register and will then have access to all the online trainings. Please make sure you list Special Olympics Arkansas when filling out the School/Association line.
Communication with Parents and Guardians
The Centers for Disease Control website www.cdc.gov/concussion provides additional resources relative to concussions that may be of interest to participants and their families.
Inclement weather policy
Rain Policy
Decisions on field closures are made as late as possible in order to give the best possible chance for the game to be played, however some decisions are easier than others and therefore it is possible that a field or park maybe closed prior to game day.
Winter Weather Policy
Players are more susceptible to injuries during cold weather, particularly from pulled or torn muscles. Players should be encouraged to wear appropriate clothing to aid body heat retention yet afford adequate movement without creating a safety hazard. As a general rule, training programs will be cancelled if the projected temperature (including wind chill) at the start of training is projected to be below 25 degrees Fahrenheit.
Hot Weather Policy
The risk of heat related illness from vigorous sports activity increases with the temperature. The body generates heat which cannot be dissipated readily when the ambient temperature exceeds 85 degrees F, depending upon the humidity. Hot weather is considered at any point where the Heat Index reaches or exceeds 100. As a general rule, training programs should be reviewed if the heat index at the start of training is projected to be above 95 degrees Fahrenheit. Coaches should exercise caution and provide additional water breaks.
Lightning and Thunder Policy
If inclement weather is forecast, an individual should be designated to monitor the weather forecast and radar during the competition. If the facility being used for competition has a lightning detection system and a facilities policy in place that is more stringent than listed below, the facilities policy will supersede Special Olympics Arkansas' policy. If lightening is detected within 10 miles of the practice or competition facility, all coaches, players, referees and spectators are to withdraw from the field and seek proper shelter. No place outside is safe near thunderstorms. The best shelter is a large, fully enclosed, substantially constructed building. A vehicle with a solid metal roof and metal sides is a reasonable second choice.
30 minutes Rule - Wait at least 30 minutes after the last sound of thunder or the last lightning flash before giving the “all clear” signal and resuming normal activity. If thunder is heard or lightning is seen again within that 30-minute time frame, the event will continue to be postponed or officials may deem to cancel the event.
Lightning research has confirmed that consecutive lightning strikes can occur as much as six miles apart. People often do not perceive lightning to be close if it is two miles or more away, but the risk of the next strike being at your location may actually be very high. Many lightning casualties occur in the beginning as a thunderstorm approaches because people ignore these precursors. When thunderstorms are in the area but not overhead, the lightning threat can exist even if it is sunny at your location.
Decisions on field closures are made as late as possible in order to give the best possible chance for the game to be played, however some decisions are easier than others and therefore it is possible that a field or park maybe closed prior to game day.
Winter Weather Policy
Players are more susceptible to injuries during cold weather, particularly from pulled or torn muscles. Players should be encouraged to wear appropriate clothing to aid body heat retention yet afford adequate movement without creating a safety hazard. As a general rule, training programs will be cancelled if the projected temperature (including wind chill) at the start of training is projected to be below 25 degrees Fahrenheit.
Hot Weather Policy
The risk of heat related illness from vigorous sports activity increases with the temperature. The body generates heat which cannot be dissipated readily when the ambient temperature exceeds 85 degrees F, depending upon the humidity. Hot weather is considered at any point where the Heat Index reaches or exceeds 100. As a general rule, training programs should be reviewed if the heat index at the start of training is projected to be above 95 degrees Fahrenheit. Coaches should exercise caution and provide additional water breaks.
Lightning and Thunder Policy
If inclement weather is forecast, an individual should be designated to monitor the weather forecast and radar during the competition. If the facility being used for competition has a lightning detection system and a facilities policy in place that is more stringent than listed below, the facilities policy will supersede Special Olympics Arkansas' policy. If lightening is detected within 10 miles of the practice or competition facility, all coaches, players, referees and spectators are to withdraw from the field and seek proper shelter. No place outside is safe near thunderstorms. The best shelter is a large, fully enclosed, substantially constructed building. A vehicle with a solid metal roof and metal sides is a reasonable second choice.
30 minutes Rule - Wait at least 30 minutes after the last sound of thunder or the last lightning flash before giving the “all clear” signal and resuming normal activity. If thunder is heard or lightning is seen again within that 30-minute time frame, the event will continue to be postponed or officials may deem to cancel the event.
Lightning research has confirmed that consecutive lightning strikes can occur as much as six miles apart. People often do not perceive lightning to be close if it is two miles or more away, but the risk of the next strike being at your location may actually be very high. Many lightning casualties occur in the beginning as a thunderstorm approaches because people ignore these precursors. When thunderstorms are in the area but not overhead, the lightning threat can exist even if it is sunny at your location.